Powerful, with a complex structure, bearing great loads, the hip joint is subject to various pathologies that lead to the onset and development of pain.

Hip pain occurs due to:
- injuries;
- infectious infection;
- destructive processes in the joints;
- inflammation;
- metabolic disorders.
A person may feel that it "gives" in the groin, buttocks, knee. Perhaps the appearance of lameness, muscle atrophy, weakness, limited functionality of the limbs.
Practice shows that the nature and intensity of the pain syndrome can be different:
- starting (until you "disperse");
- night;
- afternoon;
- constant (light, medium, strong).
Why does the leg hurt in the hip area

There are many joint and extra-articular diseases that lead to pain syndrome. Between them:
- coxarthrosis;
- arthritis of various natures;
- pseudogout;
- Kening's disease;
- fractures, dislocations, bruises;
- tendonitis;
- myositis;
- bursitis.
Pain in the hip joint: which doctor should I go to?
It is obvious that the number of pathologies that lead to hip pain or numbness cannot be treated by a specialist. Most likely, you should contact a traumatologist or rheumatologist. It is possible that consultation with a surgeon is required. Due to the fact that the pain "shoots" in the groin, buttocks, lower abdomen, a person can be referred to a neurologist. Thus, coxarthrosis "disguises itself" as sciatica, problems with nerve roots, herniated discs. But the reverse situation is also possible, when neurological pathologies are suspected, but joint disease is detected.
Women often cannot differentiate the cause of groin pain - inflammation is the appendages or joint disease. A visit to the gynecologist will bring clarity. A urologist will help men determine if there are any pathologies in the prostate gland.
diagnostic measures
In medical practice, a well-coordinated scheme has been developed, the use of which allows you to fully establish why the hip joint hurts, what to do and how to treat it.
During the first visit, the doctor's task is to collect an anamnesis. A person is asked about lifestyle, physical activity, to find out if there were any relatives with joint diseases. An external examination of the joint and its palpation are also carried out. In the presence of inflammation, this will help to narrow the circle of hypothetical diseases that cause pain.
In addition, various laboratory tests and hardware studies are assigned. As a rule, resort to:
- tomography;
- radiography;
- endoscopy.
You will need immunological and microbiological blood tests, a test for rheumatoid factor. It may be necessary to examine the synovial fluid in the joint.
treatment methods
Due to the fact that the pathologies are quite diverse, they cannot be treated according to a single scheme. For example, inflammation of the hip joint, its symptoms and treatment will differ from the work of a doctor with an injury. In case of fracture or dislocation, a rheumatologist or surgeon will prescribe joint immobilization. In infectious and purulent pathologies, it is necessary to take a course of antibiotics.
Inflammatory and degenerative diseases require the use of the following groups of drugs:
- non-steroidal;
- diuretics;
- chondroprotectors;
- muscle relaxants;
- vitamin complexes.

In this case, the treatment is long, carried out in several courses, which can last for several years. In addition to drug therapy, a person does exercises, makes efforts to lose weight, undergoes physiotherapy. If it is not possible to help the patient with conservative methods, surgical methods should be used.
How does the hip joint hurt, what symptoms characterize diseases that can cause pain, we consider traditional treatment methods. However, various joint diseases have been known to man for many thousands of years. Therefore, traditional medicine has developed a significant amount of knowledge on how to help a patient who is concerned about his joints. Of course, herbal medicines, lotions, compresses, taking decoctions and tinctures cannot be the main method of treatment, but doctors recommend it as an addition to the main therapy. He himself, without consulting a specialist, cannot drink or apply anything, as there is a danger of getting an allergy, a burn, or simply wasting time and effort without achieving results.
Treatment of pain in the hip joint with folk remedies helps to achieve an anesthetic effect, strengthens the body. Most often, alternative medicine offers public components: burdock roots, pork fat, garlic, cinquefoil, dandelion, leaves of berry bushes, buds and fruits. For example, the usual rosehip broth is a storehouse of vitamin C and an excellent diuretic that removes excess fluid and unnecessary salts, reducing the load on the legs and heart.
Pain radiates to the leg when walking - causes, symptoms
If you feel pain when walkingthighcovering the body oflower backon the lower leg or located in the hip area, you need to see a doctor. Diseases of the hip joints, which undergo high loads duringwalking, jogging, exercise classes, progress quickly and can lead to disability. In order for the movement to bring joy and benefit, monitor the health of the musculoskeletal system. If there are symptoms of pain, you need to be examined and start treatment as soon as possible. In most diseases, bone tissue, cartilage and joints are destroyed, which cannot be restored. You can only remove the inflammatory process, stop or slow down its destruction.
general description
The hip joint is multiaxial, cup-shaped. It combines the pelvis and femur into a single system, which allows a person to walk, liftlegand book. Works every step, squat. As long as the joint is healthy, we don't feel it. But with inflammation, pinchingnerves, there is severe, intense or sharp pain. It is located inthigh, but with the progression of the disease, it spreads,gives it backinsideleg, insidelower back🇧🇷
If nodeal withinflammatory process:
- the size of the joint bag is reduced, which contains synovial fluid - an intra-articular lubricant that reduces friction and slows down the wear of the joints;
- the membranes that protect the joint are damaged;
- cartilaginous, bone tissue is destroyed.
Prevention
It is possible to protect the hip joints from destruction, maintain mobility until old age, if you monitor your health. Diseases of the musculoskeletal system causes excess weight. It increases the load on the articular joints, and they wear out faster. Not only body weight in kilograms and height are important, but also the ratio of muscle and adipose tissue. Strong, trained in the gym, the muscles form a muscular corset that supports the body in an upright position, reduces the load on the spine, hip and knee joints, and feet.
The destruction of cartilage, bone tissue occurs with a lack of calcium and other trace elements. Include more vegetables, lean fish, dairy products and cheeses in the menu. Take the mineral-vitamin complexes recommended by your doctor. Avoid injuries. Do not wear uncomfortable shoes. Walk more, 2-3 times a weekDoesexercises to strengthen and stretch the muscles.
causes of pain
HipCan it beget sick🇧🇷
- after an awkward fall, blow - if the pain does not go away in 2-3 days, you need to visit a traumatologist,Doesradiography;
- with the development of arthrosis - the joint becomes inflamed, the pain is felt at rest and intensifies withwalking🇧🇷
- with arthritis - aching pain, worse at night;
- in violation of metabolism, blood flow - the tissues do not receive enough nutrients, oxygen, the removal of toxins is delayed;
- if an infection gets in - abrasions, scratches, purulent rashes on the thigh can become a gateway for infection, penetrating into the joint, causes acute infectious bursitis with unbearable acute pain;
- with diabetes mellitus, other systemic diseases;
- with inflammatory processes in the body, accompanied by fever or with a risk of spread to the joint.
It is impossible to make an accurate diagnosis on your own. For pains that do not go away for 2-3 days, you need to see a doctor,Doessearch.
varieties of pain
Acute pain in the hip joint occurs with injuries and local inflammatory processes. can start withrightorletside, but with the development of inflammation, covers the circumferencehips🇧🇷gives it backinsidelower back, insidelegs🇧🇷The doctor, after examination, will prescribe anti-inflammatory drugs that will quickly relieve pain. But sometimes it is necessary to continue treatment after its disappearance in order to remove the causes that caused the inflammation.
With severe pain, it is more difficult for a doctor to make a correct diagnosis. It can appear in one place and appear in another. If it appears periodically, you need to look at what its manifestations are connected with: at rest, withwalking, squats, sudden movements.
If pain symptoms appear for more than 6 months, the disease has become chronic. To establish the diagnosis, hardware examinations are carried out: X-ray, ultrasound, MRI,it's being doneblood analysis.
Diseases and their characteristic symptoms
pain inthighoccur with various diseases:
- bursitis;
- osteoarthritis;
- coxarthrosis;
- arthritis;
- inflammation of the ligaments;
- neuralgia.
bursitis
Bursitis is an inflammatory process in the joint bag. It is manifested by acute pain, fever, deterioration in general well-being. Under the skin, a painful, hot lump forms.cureThis disease is an orthopedic traumatologist.
osteoarthritis
A chronic disease in which the bone and cartilaginous tissues of the joint are destroyed. It develops after injuries, during menopause in women, with metabolic disorders, with excessive stress in athletes and during heavy physical work. Feeling tired in the early stageswalkingpain with sudden movementsfoot.If you start treatment at an early stage, the progression of osteoarthritis can be greatly slowed down, and motor activity can be maintained in old age. In the second stage, destructive processes in the joint affectnerves🇧🇷The pain appears in the morning and disappears in the afternoon. she candonateon your knees,lower back🇧🇷There is tissue swelling. With the progression of osteoarthritis, pain persists all the time, mobility is limited.
coxarthrosis
With coxarthrosis, the composition of the synovial fluid changes. It does not lubricate the components of the joint, and with each movement it feels severe pain, the head of the femur is displaced and deformed. The disease develops in old age or after injuries. In the initial stage, acute pain is felt withrightorletside while walking. when under deformationpinched nerves, the pain intensifies, lameness appears. in the third phaseletorrightthe leg is shortened due to the deformity of the femoral head, the difference can be 1-1. 5 cm.
Arthritis
aching pain on the outsidehipsbuttocks many consider symptomsosteochondrosis🇧🇷But when making a diagnosis, it is necessary to exclude or confirm arthritis with hardware diagnostics. Different types of arthritis are diagnosed: purulent, rheumatoid, tuberculous, psoriatic, reactive.
Inflammation of ligaments
Tenditis - inflammation of the ligaments, tendons is manifested by unbearable pain, swelling, redness of the skin, creaking when walking, fever. The inflamed tissue canpinchnerve endings, which potentiates the pain symptom. It's forbiddendeal withyour own painkillers. Such treatment can cause complications - the development of tendinosis, when the inflamed ligaments begin to collapse.
Neuralgia
If onehip hurts, leg gives wayburning pain along its lateral surface, additional tests are carried out to confirm neuralgia,pinched nerve causes🇧🇷
other symptoms
To understand whether there is a pathology in the hip joint or whether the pain is caused by the fact thatosteochondrosis in the leg, the following symptoms will help:
- when walking, running, bending over, the joint creaks or creaks;
- flexibility is lost, freedom of movement is limited - it is difficult to bend over, climb stairs, sit down;
- body temperature rises,osteochondrosisthere is no such symptom;
- gait changes;
- pain symptoms are manifested when walking, trying to get up, moving the leg, but body movements, hands do not cause discomfort.
pathology diagnosis
At theosteochondrosisand pathologies of the hip joint similar symptoms. To make an accurate diagnosis, the doctor examines the patient, clarifies the complaints, the nature and location of the pain. To determine,how to treat diseaseswhat drugs are contraindicated for the patient, additional tests are prescribed:
- blood test - shows whether there is an inflammatory process in the body, how strong it is;
- urinalysis - reveals hidden edema, disorders in the excretory system, the degree of intoxication of the body;
- blood test for the amount of fibrinogen, other nonspecific markers;
- rheumatic tests - determine the rheumatoid factor;
- proteinogram - reveals inflammatory processes, malignant and benign neoplasms, characterizes the composition of protein compounds in the blood;
- radiography - shows the condition of bones, cartilage, tendons, reveals fractures, cracks, ruptures, dislocations, the level of destruction or deformation;
- MRI or CT scan is needed to see the pathology of soft tissues: muscles, ligaments;
- Ultrasound - shows the condition of the joints, an increase in the volume of their membranes during inflammation, the presence of synovial fluid in various parts of the joint.
Features of pain treatment of different nature
There is no single scheme for the treatment of pathologies of the hip joint. Arthritis only needs meds ifpinchednerve endings are different. The doctor, after diagnosis, prescribes treatment, taking into account the stage of the disease, gender, patient age, other chronic diseases and possible allergic reactions.
Painful sensations, inflammation in arthritis are suppressed by anti-inflammatory drugs. To prevent the disease from progressing, patients take hormonal drugs. In addition to drug therapy, physiotherapy is carried out.
Bursitis is treated with nonsteroidal anti-inflammatory drugs. If the tests show a strong inflammatory process, injections are made directly into the joint. The doctor chooses an injection solution, having studied the features of the course of the disease, the general condition of the patient's body. With a high risk of complications, severe course of the disease, corticosteroid treatment is carried out.
In the early stages of coxarthrosis, treatment with anti-inflammatory drugs is effective. But if the patient did not go to the doctor when he felt thathurtsleg when walking and the disease is advanced, full or partial joint replacement is required. To restore cartilage tissue, condoprotectors are prescribed.
In pathologies of connective tissues, glucocorticosteroids are prescribed.
It is impossible to use potent drugs on your own, without a doctor's supervision. During therapy, the doctor monitors the general condition of the body, periodically prescribing blood and urine tests.
Inflamed hip joint what to do how to treat
Septic arthritis of the hip. Diagnosis and treatment
septic arthritis- a disease of childhood, and for the hip joint the average age is even lower than for arthritis in other locations: 70% of cases occur in children younger than 4 years. The smaller the child, the worse the outcome of hip arthritis. A child's refusal to walk is often associated with bacterial infections of the hip joint.
On asearch, during which the authors excluded all patients who refused to walk due to an obvious previous pathology, it was found that in 21 of the 22 patients the cause was a bacterial infection. Osteomyelitis and septic arthritis occurred with equal frequency and accounted for 14 cases out of 22. Discitis also occurred in a significant number of cases.
Increasedtemperatureit was in 82% of patients with bacterial infection, but only in 17% of those without infection. The number of leukocytes in the blood and ESR were not increased.
Pathogenesis of septic arthritis of the hip joint
At thehip septic arthritisIn the inflammatory process, Staphylococcus aureus is most often sown. The infection usually affects the joint cavity from an osteomyelitis focus within the joint capsule. Osteomyelitis, as a rule, is of hematogenous origin and affects the metaphysis of the thigh, penetrating through the supply vessels. The infection may surface in the form of a subperiosteal abscess.
Hip joint inflammationusually develops due to the penetration of the pathogen from the focus of osteomyelitis on the femoral neck into the joint capsule. There is a significant difference between the development of the disease in older and younger children. In older children, this disease is usually the result of osteomyelitis of the femoral neck. In infants, it may result from hematogenous spread in generalized sepsis.
joint cartilageit does not support the increase in intra-articular pressure caused by the pus produced by staphylococci. In addition, staphylococcus produces a staphylokinase activator, which contributes to the destruction of joint cartilage. Cartilage can withstand these forces for 4-5 days before destructive changes begin. Other organisms that can cause septic arthritis of the hip in children include pyogenic streptococcus and Pfeiffer's bacillus.
streptococcal infectionusually accompanied by a much more rapid increase in signs and symptoms. Pfeiffer's bacillus infection is usually responsible for septic arthritis that develops in children within the first 12 months of life, although it can occur in the first 2 years of life. Suspect gonococcal arthritis in young adults.

Clinical picture of septic arthritis of the hip joint
Usually,sonYou are admitted to the emergency department with a high fever, irritability, and severe pain in the affected hip joint, accompanied by significant limitation of movement in all directions and muscle spasm. The child walks with a limp or refuses to walk. The affected hip is flexed, outwardly rotated, and abducted. During the examination, the patient has pain in the groin and above the hip joint, intoxication.
Numberleukocytesin synovial fluid, on average, it is 57, 000 µl, but it can range from 10, 000 to 250, 000 µl. A shift of the formula to the left is characteristic, blood cultures are positive in more than 50% of cases. The level of mucin in the joint fluid was reduced in all cases, as was the level of glucose compared to its blood content in most of the examined patients. Erythrocyte sedimentation rate is usually increased.
In one study, all patients experienced some degree of soft tissue swelling in the hip region. The smaller the child, the more likely it is to detect joint space expansion. In another study, many patients initially had normal radiographs. The most typical was a pathological hip subluxation with widening of the joint space. Some patients had osteomyelitis of the proximal femur.
Differential diagnosis of septic arthritis of the hip
septic arthritis of the hipmust be differentiated from several other diseases. Transient synovitis can be manifested by severe pain, severe claudication and limited movement in the hip joint. Radioisotope scanning helps to differentiate this disease from septic arthritis. If it is not possible to carry out this, skin traction in the hospital bed will help to make a differential diagnosis. A significant improvement in the condition with a decrease in symptoms within 24 hours indicates transient synovitis.
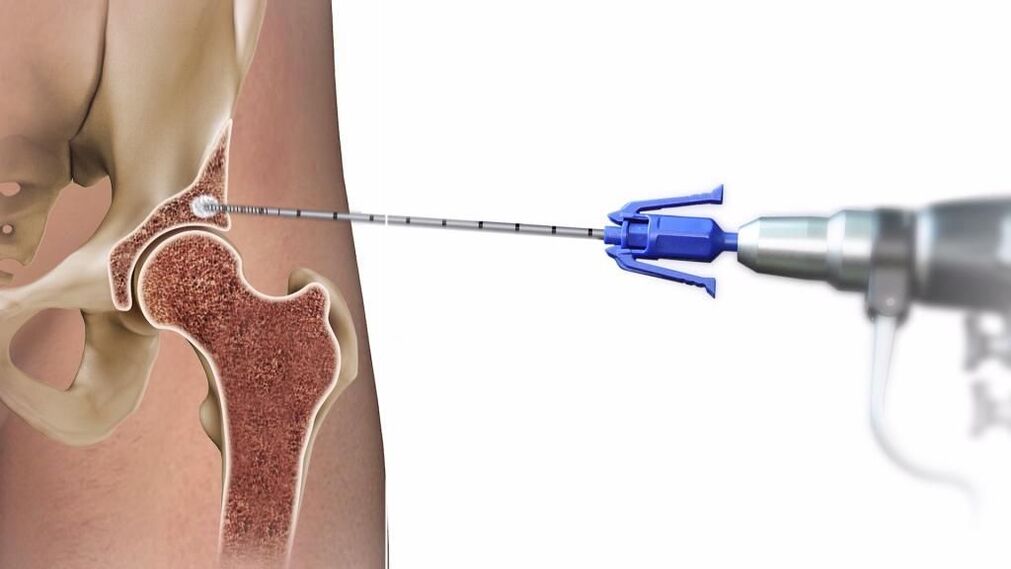
If the doctor suspectsseptic arthritis, the joint must be punctured, the effusion removed and antibiotic treatment started. Hemophilia can be difficult to differentiate, but these patients are usually registered for this disease. If this disease is suspected, urgent decompression is indicated to avoid damage to the femoral head due to increased intra-articular pressure.
rheumatic attackmay experience significant pain and limited range of motion in the hip joint. As a rule, with this disease there is volatile arthritis and arthralgia, which helps in the differential diagnosis.
Treatment of septic arthritis of the hip
perhaps the most importanttimeWhat the emergency physician should know is that the delay in diagnosing this disease and the late start of treatment worsen the prognosis and evolution of this disease. In one study, a poor outcome was observed in almost all cases when treatment was started more than 4 days after the onset of symptoms.
Purpose of treatment- removal of effusion from the joint to prevent destruction of the articular cartilage and formation of adhesions, as well as decompression of the joint to avoid impaired blood supply to the epiphysis. Adequate doses of parenteral antibiotics are required. Initially, the use of antibiotics from the penicillin group is recommended, but recently other drugs have been preferred. An important component of treatment is the puncture of the joint cavity and its washing. The physician should select the appropriate antibiotic based on the most likely suspected microorganism based on the patient's age and onset characteristics. Inoculation and Gram stain play an important role in the choice of antibiotic.
Most often foundstaphylococcal arthritis, amenable to therapy with methicillin or oxacillin. If gonococcal arthritis is suspected in adults, it is recommended to prescribe penicillin intravenously at a dose of 10 million IU / day.
Unfortunately, a way to completely get rid of coxarthrosis has not yet been invented. Even joint arthroplasty does not guarantee that dystrophic changes will stop there. Obviously, the earlier the diagnosis is made, the easier it will be to keep the disease under control and prevent relapses. With a disease at stages 1-2, it is quite possible to live and feel comfortable if you adhere to some rules and restrictions.
Treatment will only be effective after a comprehensive diagnosis. The task of treating osteoarthritis in this case is to increase the joint space, restore joint efficiency and, as far as possible, regenerate cartilaginous tissue.
If you're experiencing frequent or recurring hip pain, don't turn a blind eye to it. Is it possible to detect the disease at an early stage? You can stop the disease and prevent its development. If the doctor pleases you with the absence of a serious diagnosis, so much the better! Continue to lead a healthy lifestyle and do not forget to visit the orthopedist regularly - after all, the first alarm bell has already sounded.























